Uncategorised
Vil du være med i projektudvikling?
Patienter med rygsmerter fylder meget i almen praksis, og SDU vil gerne understøtte, at god ryghåndtering bliver nemmere. Det kræver, at vi i første omgang finder ud af, hvilke behov de praktiserende læger og deres patienter har.
Derfor er forskningsenhederne for almen praksis i samarbejde med Center for muskler og led, SDU og Diagnostisk Center ved Regionshospitalet Silkeborg gået sammen om etablering af en rygkohorte i almen praksis.
Kongressen afholdes i København til september.
DSMM's medlemmer er velkomne til at deltage.
Karen Goss er foredragsholder på kongressen.
Se mere HÉR: https://www.danskeosteopater.dk/the-4th-nordic-osteopathic-congress-2022/
Glemt kode/brugernavn
Hvis du har glemt adgangskode og/eller brugernavn til e-Bogen, kan du selv administrere dine oplysninger på vores abonnement side https://abonnement.dsmm.org/
På abonnement siden skal blot vælge LOGIN og derefter enten GLEMT DIN ADGANGSKODE eller GLEMT DIT BRUGERNAVN.
I begge tilfælde skal du indtaste din mailadresse, hvortil der så efterfølgende sendes besked.
Hilsen,
DSMM
Under afsnittet litteratur har vi samlet links til videnskabelige artikler og faglitteratur indenfor vores fagområder.
Most of our courses within the Danish Society of Musculoskeletal Medicine (DSMM) are taught in danish.
We do however provide some courses taught in english, primarily when we use foreign teachers and/or if the courses are co-sponsored by the International Federation of Manual/Musculoskeletal Medicine (FIMM) of which DSMM is a societal member.
These courses taught in englich can be attended by foreing doctors as well.
Best,
DSMM
It's a pleasure to have the opportunity to invite you to this 4-days course: Neurocranium & Cervical Spine, where Michael Kuchera, professor, DO, FAAO, will teach the subject
Manual Medicine Clinical Solutions
Neurocranium & Cervical Spine
Michael L. Kuchera, DO, FAAO
May 20-23, 2022
Munkebjerg Hotel, Vejle
COURSE ABSTRACT
Understanding key musculoskeletal, neurologic and vascular interrelationships augments both differential diagnoses and management of a wide range of clinical conditions. For a manual medicine practitioner -- informed by skilled palpation of related musculoskeletal structures, guided by physiologic knowledge, and cognizant of underlying pathophysiology -- this permits rational consideration of the value of including manual medicine approaches (or not) in patient care. Where applicable, integrating a structure/function-informed manual medicine approach often provides additional pragmatic clinical insights to mitigate pain, optimize homeostasis, reduce allostatic load and enhance overall patient health.
This course was carefully designed to enhance a structure/function-informed perspective and its application to select centralized pain syndromes, dysautonomia, and other pain or dysfunction related to head and neck structures. Many of the manual methods introduced are applicable to treatment of somatic dysfunction anywhere in the body and include soft tissue, myofascial release, balanced membranous tension (BMT) and balanced ligamentous tension (BLT), facilitated positional release (FPR), triggerpoint, and counterstrain manual techniques. Adjunctive respiratory assistance strategies will also be discussed and taught.
The course specifically emphasizes anatomical visualization, careful palpatory diagnosis and manual treatment of those musculoskeletal structures affecting the neurocranium (cranial base) and cervical spine. Significant hands-on laboratory time with both living and bony models is scheduled to maximize palpatory diagnostic hand placement and to practice manual medicine techniques. On the final day of the course, hands-on workshops will provide participants with an opportunity to reinforce the techniques taught during the course and to apply them as part of a rational, integrated sequence in mock clinical case presentations.
Goals &/or Learning Objectives
At the end of this workshop, participants will be able to:
- Visualize key anatomic inter-relationships in the cervical and neurocranial regions; understand possible pathophysiologic impact that somatic dysfunction there plays in various clinical conditions;
- Practice integration of observational and objective palpatory findings used to diagnose somatic dysfunction in these regions;
- Apply soft tissue, triggerpoint, myofascial release, balanced ligamentous/membranous, counterstrain and other manual medicine techniques to these regions with an emphasis on the neurocranium and cervical tissues;
- Understand the rationale for indications/contraindications of these various manual medicine techniques in the treated regions (and in relation to certain clinical conditions);
- Formulate a structure/function-informed manual medicine prescription to enhance health and address symptoms of the clinical conditions discussed including certain chronic centralization pain syndromes, dysautonomia, sinus and congestive headaches, temporomandibular joint dysfunction, and a variety of common clinical symptoms related to the region.
This program is part of the Danish Society of Musculoskeletal Medicine (DSMM) training for its teachers and others on the Master Course level. It is co-sponsored by the International Federation of Manual/Musculoskeletal Medicine (FIMM) of which DSMM is a societal member.
Program
Day 1
| 09:00 | Course Introduction & Pre-Test, Terminology/Landmarks. Structure/Function-Informed Models |
| 11:00 | Overview: Embryology & Developmental Anatomy of Neurocranium & Viscerocranium |
| 11:45 | Lecture: Observational & Palpatory Diagnosis of Somatic Dysfunction: Asymmetry (Static/Dynamic) |
| 12:30 | Lunch |
| 14:00 | Lab: Observational & Palpatory Diagnosis of Somatic Dysfunction: Asymmetry (Static/Dynamic) |
| 16:00 | Anatomic Visualization Part I (Bone Box – Landmarks & Relationships) |
| 17:00 | Dinner |
| 19:30 | Q&A/Craniocervical Somatic Dysfunction Diagnosis: Tenderness, Asymmetry, Restricted Motion, Tissue Texture |
| 21:00 | End Day 1 |
Day 2
| 09:00 | Review; Anatomic Landmarks and Hand-Placement for MM Diagnosis & Treatment |
| 10:00 | Types and Protocols for Delivering Various Types of Manual Medicine Technique including respiratory Assistance Strategies: Inhalation/Exhalation Phase vs Air-Hunger vs Paced Breathing |
| 11:30 | Palpatory Diagnosis & Balanced Ligamentous Tension of Cervical, Thoracolumbar, Sacral & Extremity, Somatic Dysfunctions |
| 12:30 | Lunch |
| 14:00 | Palpatory & Other MM Techniques including Facilitated Positional Release – Exemplars & Course Requests |
| 16:00 | MM Techniques for Congestive Phenomena of the Head & Neck |
| 17:00 | Dinner |
| 19:30 | Q&A/Temporomandibular Joint Dysfunction: MM Management of Involved Structures |
| 21:00 | End Day 2 |
Day 3
| 09:00 | Anatomic Visualization Part II (Self-Directed; Bone Box – Neurocranium Landmarks & Relationships) Group “Show Me” Practical Exam During Bone Box Studies (Hand-Placement, Patterns, Landmarks) |
| 10:00 | Overview Cranial Nerve Function and Dysfunction |
| 10:30 | Cranial Nerve I-II Function & Dysfunction |
| 12:30 | Lunch |
| 14:00 | CN III-VIII Function & Dysfunction |
| 16:00 | CNIX-XII Function & Dysfunction |
| 17:30 | Integration; Question-Answer-Review |
| 18:00 | End Day 3 (Festive Dinner!!!) |
Day 4
| 09:00 | Review; Question-Answer of Days 1-3 |
| 10:00 | Sinus Headaches: MM Management |
| 12:00 | Lunch |
| 13:00 | Application of Integrated MM Prescriptions for Case Simulations (including Posterior, Anterior and Cervical Headaches with additional symptoms) |
| 15:30 | Final Exam |
| 16:00 | End Day 4 |
Fee
€2,400 to be paid after you have received acceptance for taking part in the course.
The fee includes full board and lodging - except consumptions at the bar :-)
Registration
Send a mail to Peter Staehr:
The number of participants is 24.
If you're one of the first 24 signed up, you'll receive a mail with instruction for transfer of the course fee to our Danish bank.
In case of fully subscribed course, we'll establish a waiting list. If you want to be on that list just make a note on your registration.
Cancellation
Any cancellation must be made by mail to
If you cancel participation earlier than 30 days from start of the course, we'll refund you €2.100. Later cancellation will not provide a refund.
If DSMM cancel the course, e.g. due to corona, we'll refund €2.400.
Location
The course takes place at Munkebjerg Hotel on the shores of Vejle Fjord, East Jutland. 30 minutes by car from Billund Airport. Address: Munkebjergvej 125, DK-7100 Vejle, Denmark.
Read more here: https://munkebjerg.dk/en/
Ved afslutningsmiddagen på kurset Ledmobilisering fik Søren Guldager overrakt sit bevis på, at han nu er diplomlæge i DSMM - efter en god og bred muskuloskeletal uddannelse.
Stort tillykke.
Til Patienten
Har du ondt i nakke, ryg, arme eller ben?
Så er muskuloskeletal behandling måske noget for dig.
Hvad er muskuloskeletal medicin?
Muskuloskeletal medicin er udredning og behandling af smerter i bevægeapparatet (muskler, sener, led) udført af en læge.
Lægen undersøger og behandler dig med sine hænder - det kaldes manuel behandling. Du bliver også instrueret i øvelser og træning. Hvis lægen skønner, at det er nødvendigt, kan han/hun supplere behandlingen med en blokade eller akupunktur.
Hvad gør lægen?
Til jeres første møde vil lægen spørge ind til dit problem og afklare tidligere skader og behandlinger, som du har modtaget. Hvis du tidligere er blevet scannet eller har fået lavet andre undersøgelser, vil det være en hjælp, hvis du har svaret på undersøgelserne med på skrift.
Herefter bliver du grundigt undersøgt fra top til tå. Lægen ser og mærker på dine muskler, sener, led og dit bindevæv (fascier). Spændinger i muskler og fascier kan give en nedsat bevægelighed, en dysfunktion, som kan være medvirkende til dine smerter. Årsagen kan være forkert, for meget eller for lidt belastning, måske på baggrund af din holdning eller arbejdsstilling.
Hvis der ikke er andet galt, som kræver nærmere undersøgelse først, kan lægen behandle disse dysfungerende områder med manuel behandling.
Der er flere forskellige behandlingsmåder. Alle har til formål at ophæve spændinger i muskler, fascier og ledkapsler for at genoprette normal symmetrisk bevægelse i dine led.
Lægen vil ofte placere dig i en stilling, hvorfra du vil blive bedt om at aktivere dine muskler med et lille tryk eller lignende. Lægen kan også fastholde dig i en bestemt stillingen for en kortere periode, for at få smerten i et ømt punkt til at forsvinde. Ved andre behandlinger bruger lægen manipulation, som du måske kender fra kiropraktoren. Her bliver et led kortvarigt skubbet ud i en yderstilling. Sommetider kan man ved manipulationsbehandlingen høre et lille klik. Det er den samme lyd, som nogle mennesker selv er i stand til at fremkalde ved fx at trække hurtigt og kortvarigt i et fingerled.
Til sidst bliver du instrueret i relevante øvelser til at genoprette balance, styrke og bevægelighed. Øvelserne er en vigtig forudsætning for, at behandlingen kan hjælpe dig.
Eksempler på tilstande som kan behandles:
Ryg- og nakkesmerter
80% af rygsmerter har ikke en klar diagnose, som kan påvises med en scanning. Måske har du af denne grund fået at vide, at det ”bare” er muskelspændinger eller kroniske smerter, som du må lære at leve med.
Ofte drejer det sig om dysfunktioner, altså spændinger i muskler og bindevæv, som kan behandles med muskuloskeletal medicin.
Smerter i arme og ben
Kan skyldes lokale skader såsom senebetændelser, slimsækbetændelser, ledbåndsskader, slidgigt eller andre gigtsygdomme. I nogle tilfælde kan smerterne også være udstrålende smerter fra ryg eller nakke. Skaderne behandles med aflastning og træning, som stimulerer helingen og funktionen. Derudover behandles de dysfunktioner, som lægen vurderer er relateret til skaden.
Hyppige problemstillinger er indeklemningsskader i skulderen, tennisalbue, karpaltunnelsyndrom, gener efter ankelforstuvning, hælspore, nedsunken forfod og slidgigt.
Smerter i brystet
Hvis smerter i brystet ikke stammer fra de indre organer (hjerte, lunger, lever, milt, bugspytkirtel, og mavesæk) kan de stamme fra dysfunktioner i brystryggen eller ribben. Dette kan udredes og behandles med muskuloskeletal medicin.
Uforklarlige gener fra hovedet
Hovedpine, svimmelhed, kvalme, synsforstyrrelser, koncentrationsbesvær, smerter i bihuler, ører eller tænder kan stamme fra dysfunktioner højt i nakken eller over kraniet. Dette kan udredes og behandles med muskuloskeletal medicin.
Er der bivirkninger ved manuel behandling?
Det kan være, at du allerede efter første behandling mærker mindre smerter og en bedre bevægelighed i kroppen.
Men det er normalt, hvis du i en til to dage efter behandlingen også oplever en ømhed i hele kroppen og føler dig meget træt. Du kan måske blive kuldskær, svimmel, blive rød i huden, hvor du er blevet behandlet, eller opleve sveden, kvalme eller hovedpine. Du kan også opleve hyppigere vandladning og afføring. Enkelte personer reagerer med en lettere eufori på behandlingen.
Ubehaget efter behandlingen er ofte værst efter første behandling og forsvinder i løbet af et par dage.
Du kan forvente en klar bedring efter 2 - 3 behandlinger. Hvis du ikke opnår dette, må lægen vurdere din tilstand på ny. Der er ingen grund til at fortsætte en manuel behandling, hvis der ikke er en effekt.
Du må ikke have feber, når du bliver behandlet.
Hvis du lider af knogleskørhed, kræft, særlige gigtlidelser eller betændelsestilstande i kroppen, skal du sige det til lægen, som skal behandle dig.
Lægen vil da tage stilling til, om der er nogle behandlinger, du ikke skal have foretaget.
Disse forhold skal være afklaret før behandlingen starter.
Hvor får man behandlingen?
Behandlingen udføres af speciallæger, oftest praktiserende læger eller reumatologer, som har videreuddannet sig i muskuloskeletal medicin. Måske din egen læge kender behandlingen?
Her kan du finde speciallæger i dit område, som mod betaling tager imod privatpatienter.
Du behøver ingen henvisning fra din egen læge, da sygesikringen ikke giver tilskud til behandlingen. De fleste forsikringsselskaber dækker heller ikke behandlingen. Hvis du har behov for smertestillende medicin, skal du kontakte din egen læge.
Curriculum in Musculoskeletal Medicine
Danish Society of Musculoskeletal Medicine
Summary in short:
Name: DSMM
Nationality: Danish
Requirement for certification: 300 lessons required to obtain Diploma (1 lesson = 45 min)
All teaching is in person, no online teaching.
Theory teaching: 33%
Hands-on teaching: 66%
Teacher ratio: 1:6
Clinical teaching: in local groups with patients and a DSMM teacher.
Self-study: Clinical experience in own clinic (GP) or hospital and study of DSMM´s and other recommended textbooks. No control or demands.
Recognition: Musculoskeletal Medicine is recognized as additional competence by the Danish Health Authority.
Accrediting Body: DSMM´s educational board
Visions and aims of DSMM:
- To spread the knowledge of Musculoskeletal Medicine to all Danish Medical Doctors.
- To integrate Musculoskeletal Medicine into the general health system in Denmark.
Musculoskeletal Medicine, MM, is the knowledge of and skills in diagnosis, treatment and prevention of reversible dysfunctions in the neuro-musculoskeletal system. Atraumatic therapies and exercise are used to correct dysfunctions in the muscles, joints and surrounding structures. The aim is to restore maximal painless movement and postural balance.
Teachers:
The teachers of DSMM undertakes all muskuloskeletal training of Medical Doctors in Denmark.
All teachers have achieved a 300 lessons Diploma and most teachers have many years teaching experience in Musculoskeletal Medicine.
The teachers are expected to maintain their professional knowledge at the Master courses, Annual Meetings and International Congresses.
New teachers participate in the Teachers Education Programme:
- After 200 lessons you can become assistant on the Columna course (Basic course) - after appointment by the chairman of Education Committee.
- The chairman of Education Committee performs a personal education plan. You have to agree to the terms of your plan.
- You need to participate as an assistant in several courses, appointed by the chairman of the education committee.
- You can start teaching with an experienced teacher at your side, when you have obtained the 300 lessons Diploma and have worked as an assistant as pointed out in your personal education plan.
- To further develop skills as a teacher you have to participate as an assistant, before you can take on the task of teaching on that specific course.
Certification:
Diploma in Musculoskeletal Medicine
In order to be awarded a diploma in musculoskeletal medicine, it is expected that you:
- are a member of DSMM
- have a Danish medical specialist authorization in a recognized specialty
- are familiar with the theoretical knowledge behind musculoskeletal medicine
- can recognize range of movement of the individual joints incl. the joints in the entire columna
- can treat dysfunctional joints with both direct and indirect treatment techniques
- can diagnose muscular imbalance
- can treat tight postural muscles
- can give the instructions in relevant home exercises
Educational requirements for awarding a diploma in musculoskeletal medicine:
- 300 lessons, completed within the last 15 years
- completed all courses in the Danish Syllabus
- attended at least 2 annual meetings / congresses in musculoskeletal medicine
- Participating in bedside teaching of musculoskeletal medicine in local groups with patients and a DSMM teachercan account with a maximum of 66 lessons.
- Other relevant courses / meetings can be recognized - after a concrete assessment by the chairman of the education committee. Can account for a maximum of 49 lessons.
Requirements for recertification of diploma status:
The diplomat undertakes to maintain his / her competences by participating in min. 2 courses among the courses of DSMM within 5 years, one of which must be a Mastercourse.
The Danish Syllabus in Musculoskeletal Medicine:
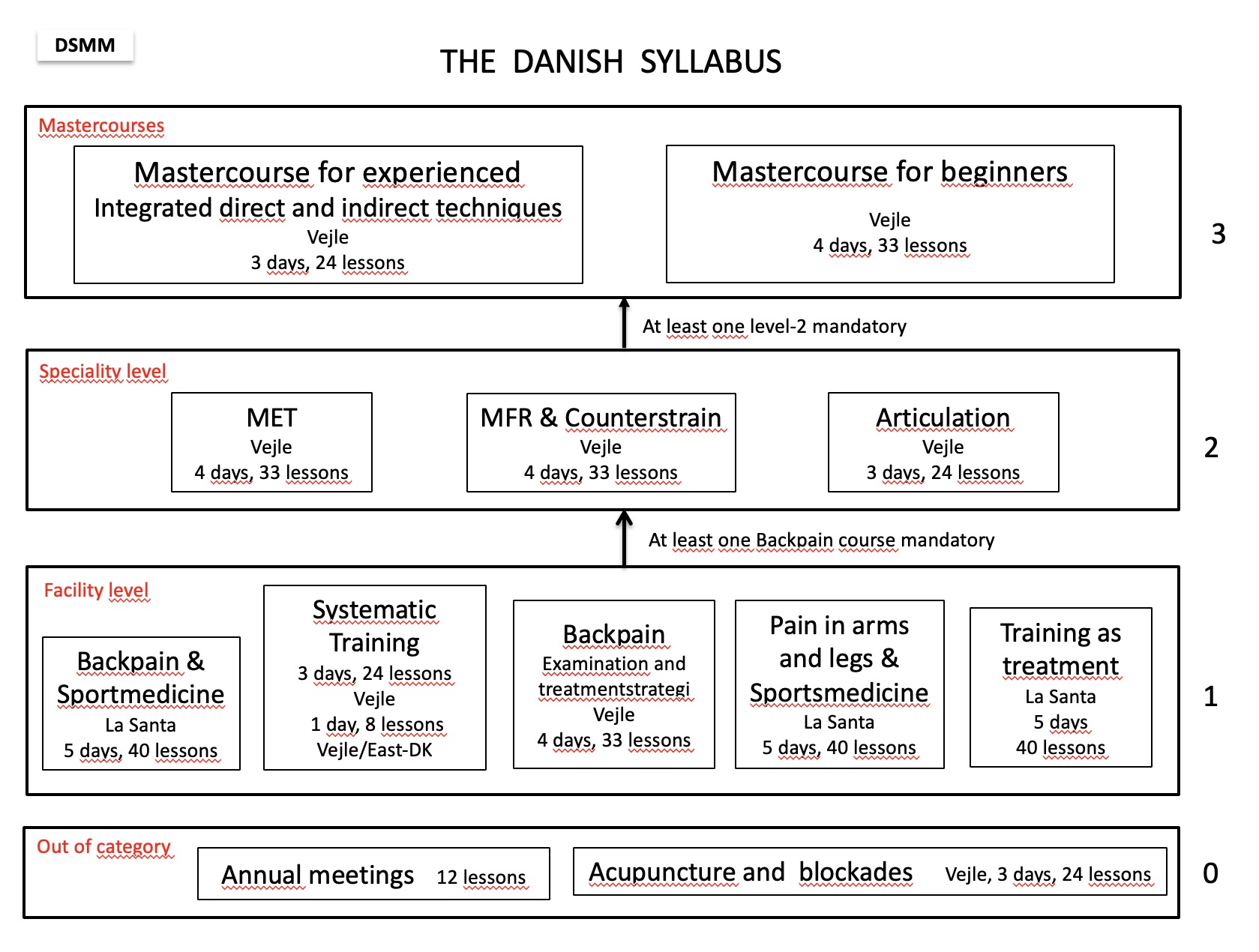
Figure 1.
Facility level: 104 lessons
Speciality level incl. Mastercourse: 211 lessons
Total programme: 315 lessons
Abstracts of DSMM´s courses, as presented on www.dsmm.org:
Facility level:
Systematic Training, “The Diagnostic challenge”
(3 days – 24 lessons)
We take you through the diagnostic process with unspecific symptoms incl. the vegetative symptoms.
We combine examination techniques with the diagnostic process to get the right diagnoses, to be aware of the sick people, and let the healthy remain healthy.
After this course, you have gained knowledge of the diagnostic process from the patient's symptoms to the choice of the right examinations including paraclinical examinations and imaging. What is the most likely diagnosis? After this course you are well prepared to give an explanation and treatment plan to your patient.
Columna course or Columna and Sports medicine
2 almost identical basic courses in Musculoskeletal Medicine
(4 days – 33 lessons or 5 days - 40 lessons)
The course gives you an overview and makes it easier to work with the musculoskeletal system in a busy working day.
The course is the compulsory basic course on the subject musculoskeletal medicine. You learn to examine and treat back pain, as well as being taught to diagnose shoulder and muscular imbalances around the hip and pelvic girdle. Through theoretical presentations and repetitive training you will acquire practical skills in diagnostics, soft tissue treatment and other modalities, which you can apply in your practice immediately after the course.
These are the patients that you will be better able to help after this course: Patients with pain in the neck, thorax, hip, lumbar and shoulder, besides patients with headache, dizziness and whiplash symptoms. All of these are diseases and dysfunctions of the musculoskeletal system and a very large area of concerns in general practice.
In addition to this the course in Columna and Sports medicine will address the most frequent sports injuries in the musculoskeletal system. You will be taught training physiology and get control of the examinations and treatment techniques of acute and stress induced sports injuries. We will go into rehabilitation and exercise treatments via a brand new app with interactive training programs for the most frequent disorders of the musculoskeletal system.
After completing one of these Basic Courses in Musculoskeletal Medicine, you will be able to attend courses at the Speciality level, in the order as shown in the Syllabus or continue courses at the facility level.
Extremity course
(5 days - 40 lessons)
This is a new course at Facility level and still on planning. We expect the first course will be in 2020. We are planning to work our way through the joints with theory, tests, diagnostics and treatment methods.
Annual meetings
(2 days – 10 lessons)
A mixture of lectures and workshops with a specific topic related to Musculoskeletal medicine. The topic is changing from year to year.
All medical doctors, physiotherapists and chiropractors are welcome.
Speciality level:
Counterstrain and MFR A - Counterstrain and Myofascial Release Technique A
(3 days - 24 lessons)
Counterstrain, CST, and Myofacial Release, MFR, are two gentle therapies that aim to give the patient an immediate pain relief. CST is an indirect technique, where you work away from the restrictive barrier to a "balance point" with the least possible tissue strain in all levels. By passive positioning the patient a reduction in the inappropriate proprioceptive activities in the dysfunctional area - and thereby pain relief - is achieved. MFR is based on the tissue's viscoelastic and neuromuscular properties, and can be used against the barrier or away from it.
On this course your ability to feel tension in the tissue gets optimized.
Both treatment methods can be used for very acute patients where other treatments is not possible. But the techniques are also extremely useful for patients with chronic muscular pain, osteoporosis or pain around scars.
This course deals primarily with columna and costae.
Counterstrain and MFR B - Counterstrain and Myofascial Release Technique B
(3 days – 24 lessons)
This course is a continuation of the Counterstrain and MFR A course and, in addition to repetition and optimization of some of the techniques from Counterstrain and MFR A, it also deals with examination and treatment of the extremities all the way from the hip and pelvis to the feet and from the shoulder to the hand.
After this course you can apply the CST and MFR concepts in all regions.
It is a requirement that the Counterstrain and MFR A course are completed.
MET A, Muscle Energy Technique A
(4 days - 33 lessons)
This course is an extension of the Columna course. You will learn to master the functional diagnostics and treats with MET.
The technique is gentle and atraumatic. At the MET A course we are focused on the biomechanical and neurophysiological background for the treatment technique, as well as on the diagnosis and treatment of dysfunctions throughout the spine including the ribs.
These are the patients that you will be better able to help after this course: Patients with headache, upper cervical syndrome, thoracic pain, and patients with cardiac, gastrointestinal and urogenital symptoms due to muscular dysfunction.
MET A is the first course in a series of courses and is followed by MET B.
MET B, Muscle Energy Technique B
(4 days - 33 lessons)
MET B is a continuation of the MET A course. In addition to repetition and optimization of some of the techniques from MET A this course deals with diagnostics and treatment of the extremities and the pelvic girdle. The concepts can then be used in all the regions of the body.
Beside dealing with Muscle Energy Techniques, you will be introduced to the manipulation technique HVLA, High Velocity Low Amplitude for the first time.
The symptoms you will be able to diagnose and treat better after the course includes: Pelvic pain, pelvic pain in pregnant women, shoulder pain, tennis and golf elbow, recurrent sprains and pain in the foot.
It is a requirement that the MET A course is completed.
MET and Manipulation
(4 days - 33 lessons)
This course is a combined course and a graduation course for the MET courses. It is based on our daily life, where a MET treatment just lack the last "little notch" - the HVLA manipulation - in order to succeed. The course will focus on learning and implementing the various manipulation techniques that can be used with advantage in the interaction with MET. It is a requirement that the MET B course is completed.
After this course you will be even better at working in a natural flow with test and treatment for the benefit of you and your patients.
Sports and overload injuries
(5 days - 40 lessons)
This course builds on a neurophysiological exercise concept and includes diagnostics and treatment techniques that can be used both in general practice and in the field of sports medicine. The pain embossed or injured patient can be evaluated and treated solely on the basis of this concept, which is based on Janda's principles of tight postural and weak phasic muscles. In addition, an assessment of the entire overall motor control of the individual muscles and muscular dysfunctions is taught.
Exercise therapy is the basis for all post-treatment of musculoskeletal disorders and can serve as a relapse prophylaxis. In 2017, a new course material was prepared with pictures and description of the home exercises. The course participants get the exercises handed out on a USB key just to print specific exercises to the patients.
In this course we also teach risks and damage mechanisms in connection with our patients' exercise and sports activities. La Santa is chosen as a course venue, because the facilities of the place allow the course participants to gain practical knowledge of biomechanical conditions, movement patterns and, not least, injuries during the exercise of different types of sports. Completed both MET A andCounterstrain and MFR A is a requirement for participation in the Sports and overload injuries course.
Mastercourse - Integrated direct and indirect techniques
(3 days - 24 lessons)
This course is an integrated mastercourse where all treatment techniques are mixed and the treatments will look like our daily life as much as possible. The topics are different from course to course. Currently we have a series of courses with Michael Kuchera from the USA. The courses can be taken independently of each other. See the announcement of the current course.
In order to participate at the Mastercourse, it is recommended that you have completed all the courses at the Specialty level. If you are unsure whether you are ready to participate in the Mastercourse, contact the chair of the educational committee.
The broad overview of DSMM´s curriculum contains the following:
- Functional anatomy and biomechanics of the locomotor system
- Physiology and pathophysiology of the locomotor system
- Principles of MM medicine and major postulated mechanisms of action
- Anatomy, physiology and pathophysiology of the nervous system in relation to pain and dysfunction
- Specific postulated mechanisms of MM medicine diagnostic and therapeutic techniques
- Clinical syndromes and differential diagnostics of the locomotor system
- Relevant ancillary diagnostics (e.g. laboratory-, imaging-, electro-diagnostics) to MM medicine
- Risks and benefits of other relevant therapeutic modalities compared to or in conjunction with manual medicine
- Indications and contraindications for different therapeutic options
Detailed curriculum:
In all courses theory and practical training are integrated. The differentiations of the below in different skills are an estimate.
The main frame of the training sessions is: screening, scanning, treatment, re-examination and instruction in specific exercise or general training.
The Scanning, treatment and re-examination are performed as a flow from part of examination to specific treatment to re-examination. An example of this is while we do the provocation test, we treat addressing the resistance and immediately after make a re-test for the range of motion.
Essential skills:
- Informing the patent adequately about their condition in order to obtain informed consent
- Effectively inform the patient about anticipated benefits and outcomes, potential risks and complications of MM treatments
- Applying affective, cognitive, and psychomotor skills to conduct effective history taking and physical examination
- Applying affective, cognitive, and psychomotor skills to conduct effective, accurate palpatory diagnosis
- Applying knowledge and competence to deliver safe, effective MM medicine treatment in a general population
- Applying knowledge and competence to deliver safe, effective MM medicine treatment in complex morbidity or special musculoskeletal complaints
Columna course 1,3 lessons
Extremities 1 lesson
MET A 1 lessons
CST-MFR A 2,3 lessons
CST-MFR B 0,5 lessons
Sports medicine 1 lesson
Mastercourse 2 lessons
Anatomy, Physiology and Evidence:
- To comprehend and to describe the normal functions of the muscles and joints of the axial and appendicular skeleton, and the function of the nervous system as it pertains to the functions of the locomotor system
- To understand the anatomical basis of techniques used to investigate and manage complaints of the locomotor system
- To evaluate critically the established and new theories on the pathogenesis, mechanisms and management of complaints regarding the locomotor system
- To describe macrostructure, anatomical relations and surface anatomy of the elements of the locomotor system, including bones, joints, intraarticular inclusions, bursae, ligaments, muscles, tendons, entheses, fasciae and nerves
- To understand the principles of tensegrity
- To describe the attachments and actions of muscles related to the main syndromes of the locomotor system
- To describe the course and relation of the peripheral arteries (especially the vertebral arteries) and the effects on these vessels of movements of the associated skeletal structures
- To state the peripheral and segmental nerve supply of muscles and joints related to the main musculoskeletal syndromes
- To describe and demonstrate the course and distribution of the peripheral and autonomic nerves in a detail appropriate to the interpretation of musculoskeletal complaints and the comprehension of investigations involving these nerves as they pertain to musculoskeletal complaints
- To describe the disposition and attachments of all the structures within the vertebral canal, and the effects on these structures of movements of the vertebral column, head and limbs
- To describe the basic neuroanatomy to explaining the motor and sensory mechanisms involved in movements and musculoskeletal complaints
- To recognize anatomical variants in neural and musculoskeletal structures
- To describe muscle adaptability
- To distinguish the ability of postural and phasic muscles
- To describe the effects of rest, exercise and ageing on skeletal muscle, in terms of histochemistry and molecular structure
- To describe the neurophysiology, activity and function of reflexes involving the locomotor system including somato-visceral, viscera-somatic, and somato-somatic relationships
- To describe the effects of rest, exercise and ageing on fascia, in terms of histochemistry and molecular structure
Columna course 4 lessons
Extremities 5 lessons
MET A 4 lessons
MET B 1 lesson
CST-MFR A 1,3 lessons
CST-MFR B 2,7 lessons
Sports medicine 1 lesson
Presumed knowledge from pre-graduate studies:
- To describe the anatomical basis of mechanotransduction
- To describe different types of muscular fibres
- To describe the basic metabolic principles and physiology of bone, muscle, connective tissue and nerves pertaining to the locomotor system
- To describe the molecular and cellular processes implicated in mechanisms of muscle contraction
- To describe the molecular and cellular processes involved in the generation and propagation of action potentials in nerve, muscles, and excitatory and inhibitory synapses
Biomechanics:
- To understand certain precepts of biomechanics and apply them to the locomotor system
- To recognize and describe the aberrations of function of the locomotor system
- To define, in biomechanical terms, the following terms as they are applied to joints: hypomobility, hypermobility and instability
- To describe biomechanical differences between capsular and somatic dysfunction and capsular patterns
- To demonstrate an ability to apply and interpret the following terms with respect to any of the tissues of the locomotor system: stress, strain, stiffness, toughness, viscoelasticity, creep, hysteresis and fatigue failure
- To describe the movement of any joint in terms of translation and rotation about biomechanical axes
- To demonstrate an ability to apply precepts of biomechanics to clinical features, posture, the gait cycle, and activities of daily living, including occupational and recreational activities
Columna course 3,2 lessons
Extremities 2 lessons
MET A 3 lessons
MET B 2 lessons
CST-MFR A 0,4 lessons
Sports medicine 4 lessons
Pain physiology, acute and chronic manifestations:
- To understand the physiology of pain and the pathophysiologic and biopsychosocial implications of pain
- To understand the somatic and visceral structures which contain receptors capable of creating pain
- To describe, at an appropriate level, the taxonomy of pain
- To differentiate acute and chronic pain and their proposed mechanisms
- To describe the anatomy, physiology, pathophysiology, and currently understood mechanisms of pain
- To describe the understood patterns of referred pain to and from the locomotor system
- To describe the relationship between psychosocial factors and chronic pain
- To describe the role of the autonomic nervous system in relation to pain
Columna course 1 lesson
Extremities 1 lesson
MET A 2 lessons
CST-MFR A Totally integrated
CST-MFR B Totally integrated
Sports medicine 1 lesson
Integration of MM with medical examination:
- To perform a conventional medical examination to understand the condition of the patient with respect to indications, contraindications and therapeutic options
- To perform thorough history and examination with emphasis on biomechanical, occupational, orthopaedic, neurological, biopsychosocial factors, to inspect posture, gait, and gross ranges of motion
- To perform orthopaedic, neurological, systemic and ancillary tests where indicated
- To prioritize diagnostic tests based on sensitivity, specificity and cost-effectiveness
- To describe practice guidelines or critical pathways in sequencing diagnostic evaluation for the patient
Systematic Training 16 lessons
Manual medicine examination and evaluation, the main frame of all courses:
- To perform screening examination to identify if there is a problem in the locomotor system that deserves additional evaluation
- To perform a scanning examination to identify which regions and tissues within the region are dysfunctional and of relevance at a level appropriate to the treatment skills
- To conduct regional palpatory examinations of the tissues of the locomotor system to identify dysfunctions
- To conduct palpatory examinations of local tissues to determine the specific dysfunctions considered for MM treatment and the characteristics important in the selection of the treatment modality including indications and contraindications
- To conduct different palpatory examinations in order to look at and record elements of pain provocation, sensory changes, tissue texture changes, examination of range of motion, and Characteristics of end feel barrier.
Using STAR (Sensory change, Tissue texture abnormality, Asymmetry, Range of motion) and MIP (Mobilisation, Irritation, Provocation) as mnemonics.
Columna course 3 lessons
Extremities 8 lessons
Systematic Training 8 lessons
MET A 3,5 lessons
MET B 5 lessons
CST-MFR B 2,3 lessons
MET-Manipulation 2,5 lessons
Sports medicine 3 lessons
Mastercourse 4 lessons
Diagnostic technology, evaluation of treatment, re-testing:
- To record the patient evaluation and patient progress by using various methods of measurement
- To record relevant specific findings in terms of MM medicine
Columna course 4 lessons
Extremities 2 lessons
MET A 1 lesson
MET B 1 lesson
CST-MFR A Totally integrated
CST-MFR B 1,5 lessons
Sports medicine 4 lessons
Presumed knowledge from the postgraduate medical specialist education:
- To record pertinent related outcomes measures e.g. visual analogue scale (VAS), dolorimeter, impairment scales, general health scales
Types of modalities of treatment:
DSMM´s courses cover the following modalities of treatment.
- Soft Tissue technique.
- Myofacial Release technique (MFR).
- Mobilisation without impulse.
- Neuromuscular therapy (Muscle Energy Technique, MET).
- Mobilisation with impulse (HVLA, High Velocity Low Amplitude thrust technique).
- Integrated techniques (Indirect Functional Techniques).
- Balance and Hold.
- Dynamic Functional Procedures. operator active.
- Dynamic Functional Procedures. operator passive.
- Release by positioning (Counterstrain)
- Integrated techniques at the cranium.
- To conduct mobilisation techniques including specific techniques for muscle inhibition or muscle relaxing (muscle energy techniques, techniques based on post isometric relaxation and on reciprocal inhibition, and positioning techniques)
- To conduct segmental manipulation techniques of the spine and the peripheral joints
- To supervise or monitor physiotherapy and training for rehabilitation
- To conduct myofascial techniques
- To conduct trigger point therapy
- To apply treatment strategies for interlinked functional (chain reaction) syndromes
- To integrate the principles of treatment of MM medicine into multimodal treatment concepts
Columna course
Mobilisation without impulse, introduction to MET 12,5 lessons
Extremities
Mobilisation without impulse, introduction to MET 17 lessons
MET A 15 lessons
MET B
MET 19 lessons
HVLA 5 lessons
MET and Manipulation
MET 16 lessons
HVLA 15 lessons
CST-MFR A
CST 12 lessons
MFR 6 lessons
CST-MFR B
CST 12 lessons
Indirect Functional Techniques 1 lesson
MFR 3 lessons
Sports medicine
Mobilisation without impulse, MET 3 lessons
Mastercourse
All modalities 18 lessons
Disease prevention and health promotion:
Exercise and training according to the musculoskeletal ailment.
- To use all treatment modalities to prevent recurrence of presenting problems in MM medicine
- To maximise biomechanical and physiological functions in activities of daily living, in activities in work and in sports
- To recommend exercise and sound ergonomic behaviour for rehabilitation and prevention
Columna course 2 lessons
Extremities 4 lessons
CST-MFR B 1 lesson
Sports medicine 14 lessons
|
MM approach in clinical pictures (syndromes):
|
Columna course 2 lessons
MET A 3,5 lessons
MET B Totally integrated
CST-MFR A 2 lessons
CST-MFR B Totally integrated
Sports medicine 9 lessons
Curriculum i Muskuloskeletal medicin
Dansk Selskab for Muskuloskeletal Medicin, DSMM
Formål og Vision for DSMM:
- At udbrede kendskab til muskuloskeletal viden til danske læger
- At få integreret muskuloskeletal medicin i det danske sundhedsvæsen
Muskuloskeletal medicin, MM, er viden om og færdigheder i diagnostik, behandling og forebyggelse af reversible dysfunktioner i det neuro-muskuloskeletale system. Der benyttes atraumatiske behandlingsformer og øvelser, der korrigerer dysfunktioner i muskler, led og omkringliggende strukturer med det formål at genoprette maximal smertefri bevægelighed i postural balance.
Lærere:
DSMM´s lærere er ansvarlig for undervisningen af danske læger i MM
Lærerkrav:
- Fuldt uddannelse som diplomlæge i MM med min. 300 lektioner
- Pædagogisk kompetence
- Det forventes at lærerne holder deres faglige viden vedlige på Masterkurser, Årsmøder, Lærermøder og Internationale kongresser
- Som underviser på La Santa kurser:
- Assistent på Ryg og idrætsmedicin eller Ekstremitetskursus forudsætter, at man har undervist på mindst 2 Rygkurser i Danmark
- Assistent på Idræts og overbelastningsskader forudsætter, at man har undervist på mindst 2 Rygkurser i Danmark - og været assistent eller lærer på MET A og B samt CST-MFR A og B
- Tvivlstilfælde afgøres af Uddannelsesudvalgsformanden
Assistentkrav:
For at komme i betragtning som assistent/lærer gælder følgende:
- Assistenten skal have min. 200 lektioner i DSMM´s Uddannelsesplan i MM
- Assistenten skal godkendes af Uddannelsesudvalget
- Uddannelsesudvalgsformanden laver en personlig uddannelsesplan
- Assistenten skal godkende sin uddannelsesplan
- Assistenter og lærere får kurser til kostprisen
- Man skal være Diplomlæge før man kan undervise som lærer
Grundregler for Assistenternes uddannelsesplan:
- Man skal deltage i alle DSMM´s kurser som kursist
- På alle kurser - på nær Rygkursus - underviser man allerede fra første gang som assistent til assistentløn
Certifikat:
Diplom i Muskuloskeletal Medicin:
For at få tildelt diplom i muskuloskeletal medicin forventes det, at man er medlem af DSMM og har dansk speciallægeautorisation i et anerkendt speciale, samt at man som minimum:
- Er fortrolig med den teoretiske viden bag muskuloskeletal medicin
- kan registrere frihedsgrader i bevægelse af de enkelte led inkl. leddene i hele columna
- kan behandle dysfungerende led med såvel direkte som indirekte behandlingsteknikker
- kan diagnosticere muskulær ubalance
- kan udspænde stramme posturale muskler
- kan instruere i relevante hjemmeøvelser
Uddannelseskrav for tildeling af diplom i muskuloskeletal medicin:
- 300 lektioner gennemført indenfor de sidste 15 år
- Ansøgeren skal have deltaget i alle kurser i uddannelsesplanen Diamanten
- Ansøgeren skal have deltaget i mindst 2 årsmøder/kongresser i muskuloskeletal medicin
- Undervisning i muskuloskeletal medicin i DGE-regi, hvor der er en DSMM-lærer som underviser, regnes med - dog maksimalt med 66 lektioner
- Funktion som underviser i muskuloskeletal medicin i DSMM-regi regnes med, dog maksimalt med 66 lektioner
- Andre relevante kurser/møder i andet regi kan indregnes – efter konkret vurdering af uddannelsesudvalgsformanden. Kan maksimalt tælle 49 lektioner
Krav til opretholdelse af diplomlæge status:
Diplomlægen forpligter sig til at vedligeholde sine kompetencer ved at deltage i min. 2 kurser i DSMM regi inden for 5 år, hvoraf det ene skal være et Masterkursus.
Dansk pensum i Muskuloskeletal medicin:
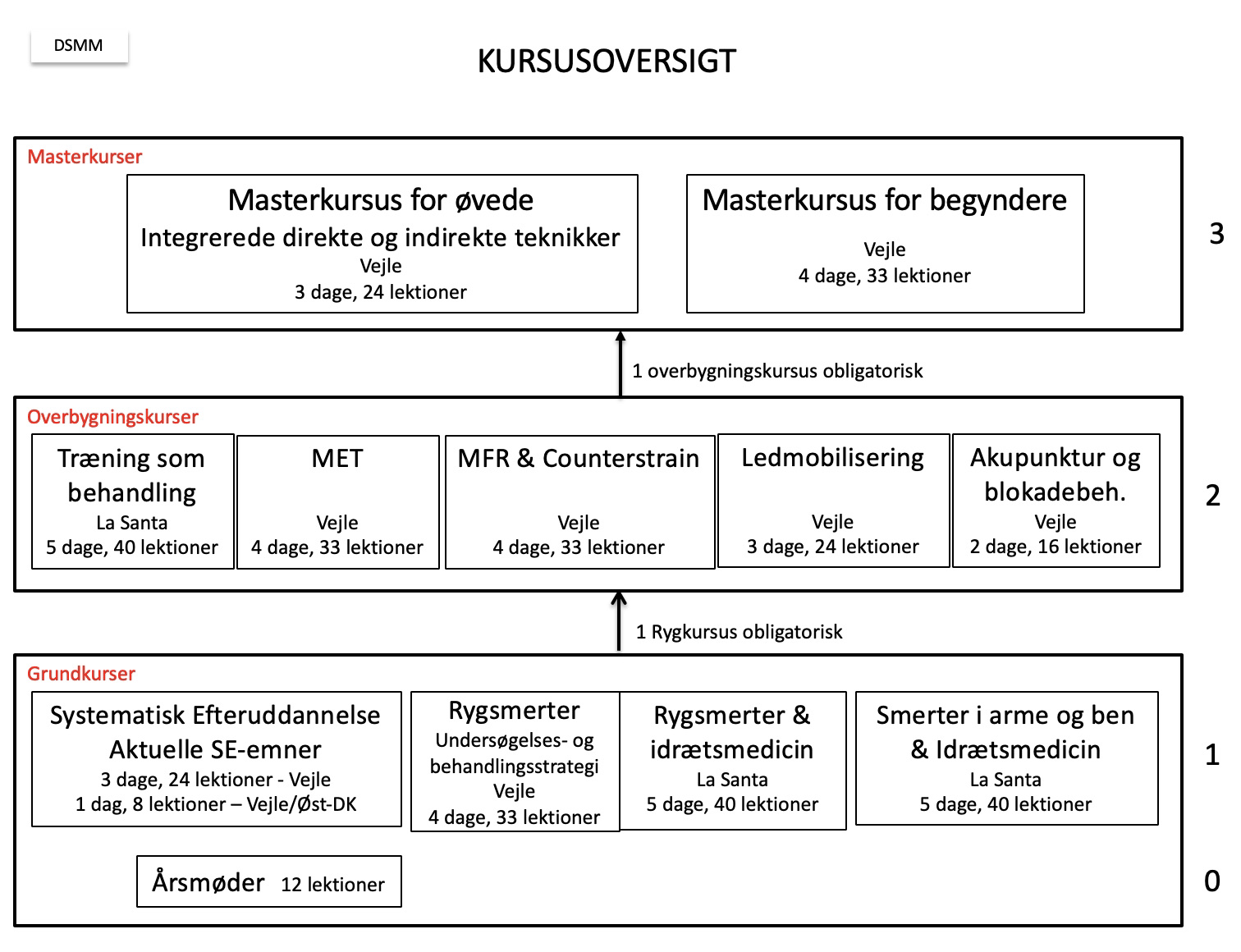
Grundkurser 104 lektioner
Overbygningskurser 211 lektioner
I alt ved gennemført samtlige kurser 315 lektioner.
Curriculum:
Overordnet indeholder vores kurser følgende, som opfylder FIMM’s krav:
- Functional anatomy and biomechanics of the locomotor system
- Physiology and pathophysiology of the locomotor system
- Principles of MM medicine and major postulated mechanisms of action
- Anatomy, physiology and pathophysiology of the nervous system in relation to pain and dysfunction
- Specific postulated mechanisms of MM medicine diagnostic and therapeutic techniques
- Clinical syndromes and differential diagnostics of the locomotor system
- Relevant ancillary diagnostics (e.g. laboratory-, imaging-, electro-diagnostics) to MM medicine
- Risks and benefits of other relevant therapeutic modalities compared to or in conjunction with manual medicine
- Indications and contraindications for different therapeutic options
Detaljeret Curriculum:
I alle kurser er teori og praktisk træning integreret. Adskillesen nedenfor i forskellige færdigheder er derfor et skøn.
Træningsdelen i alle kurser bygger på samme undersøgelses- og behandlingsramme: screening, scanning, behandling, re-test og instruktion i specifik træning eller almen træning.
Undersøgelse og behandling udføres i et bredt omfang ud fra samme greb, ”Sjalsgrebet”, som kan udføres med patienten i stående eller siddende stilling. Det tilstræbes at undersøge og behandle med færrest mulige stillingeskift.
Grundlæggende forudsætninger for objektiv vurdering:
Anamnestiske oplysninger der belyser kontraindikationer, information til patienten om forventede bivirkninger og indhentning af informeret samtykke fra patienten.
Rygkursus 1,3 lektioner
Ekstremitetskursus 1 lektion
MET A 1 lektion
CST-MFR A 2,3 lektioner
CST-MFR B 0,5 lektioner
Idræts- og overbelastningsskader 1 lektion
Masterkursus 2 lektioner
Opfylder FIMM’s krav:
- Informing the patent adequately about their condition in order to obtain informed consent
- Effectively inform the patient about anticipated benefits and outcomes, potential risks and complications of MM treatments
- Applying affective, cognitive, and psychomotor skills to conduct effective history taking and physical examination
- Applying affective, cognitive, and psychomotor skills to conduct effective, accurate palpatory diagnosis
- Applying knowledge and competence to deliver safe, effective MM medicine treatment in a general population
- Applying knowledge and competence to deliver safe, effective MM medicine treatment in complex morbidity or special musculoskeletal complaints
Anatomi , Fysiologi og Evidens:
Rygkursus 4 lektioner
Ekstremitetskursus 5 lektioner
MET A 4 lektioner
MET B 1 lektion
CST-MFR A 1,3 lektioner
CST-MFR B 2,7 lektioner
Idræts- og overbelastningsskader 1 lektion
Opfylder FIMM´s krav:
- To comprehend and to describe the normal functions of the muscles and joints of the axial and appendicular skeleton, and the function of the nervous system as it pertains to the functions of the locomotor system
- To understand the anatomical basis of techniques used to investigate and manage complaints of the locomotor system
- To evaluate critically the established and new theories on the pathogenesis, mechanisms and management of complaints regarding the locomotor system
- To describe macrostructure, anatomical relations and surface anatomy of the elements of the locomotor system, including bones, joints, intraarticular inclusions, bursae, ligaments, muscles, tendons, entheses, fasciae and nerves
- To understand the principles of tensegrity
- To describe the attachments and actions of muscles related to the main syndromes of the locomotor system
- To describe the course and relation of the peripheral arteries (especially the vertebral arteries) and the effects on these vessels of movements of the associated skeletal structures
- To state the peripheral and segmental nerve supply of muscles and joints related to the main musculoskeletal syndromes
- To describe and demonstrate the course and distribution of the peripheral and autonomic nerves in a detail appropriate to the interpretation of musculoskeletal complaints and the comprehension of investigations involving these nerves as they pertain to musculoskeletal complaints
- To describe the disposition and attachments of all the structures within the vertebral canal, and the effects on these structures of movements of the vertebral column, head and limbs
- To describe the basic neuroanatomy to explaining the motor and sensory mechanisms involved in movements and musculoskeletal complaints
- To recognize anatomical variants in neural and musculoskeletal structures
- To describe muscle adaptability
- To distinguish the ability of postural and phasic muscles
- To describe the effects of rest, exercise and ageing on skeletal muscle, in terms of histochemistry and molecular structure
- To describe the neurophysiology, activity and function of reflexes involving the locomotor system including somato-visceral, viscera-somatic, and somato-somatic relationships
- To describe the effects of rest, exercise and ageing on fascia, in terms of histochemistry and molecular structure
Forudsat prægraduate viden fra Universitetet:
- To describe the anatomical basis of mechanotransduction
- To describe different types of muscular fibres
- To describe the basic metabolic principles and physiology of bone, muscle, connective tissue and nerves pertaining to the locomotor system
- To describe the molecular and cellular processes implicated in mechanisms of muscle contraction
- To describe the molecular and cellular processes involved in the generation and propagation of action potentials in nerve, muscles, and excitatory and inhibitory synapses
Biomekanik:
Rygkursus 3,2 lektioner
Ekstremitetskursus 2 lektioner
MET A 3 lektioner
MET B 2 lektioner
CST-MFR A 0,4 lektioner
Idræts- og overbelastningsskader 4 lektioner
Opfylder FIMM´s krav:
- To understand certain precepts of biomechanics and apply them to the locomotor system
- To recognize and describe the aberrations of function of the locomotor system
- To define, in biomechanical terms, the following terms as they are applied to joints: hypomobility, hypermobility and instability
- To describe biomechanical differences between capsular and somatic dysfunction and capsular patterns
- To demonstrate an ability to apply and interpret the following terms with respect to any of the tissues of the locomotor system: stress, strain, stiffness, toughness, viscoelasticity, creep, hysteresis and fatigue failure
- To describe the movement of any joint in terms of translation and rotation about biomechanical axes
- To demonstrate an ability to apply precepts of biomechanics to clinical features, posture, the gait cycle, and activities of daily living, including occupational and recreational activities
Smerte fysiologi, akut og kronisk dysfunktion:
Rygkursus 1 lektion
Ekstremitetskursus 1 lektion
MET A 2 lektioner
CST-MFR A helt integreret
CST-MFR B helt integreret
Idræts- og overbelastningsskader 1 lektion
Opfylder FIMM’s krav:
- To understand the physiology of pain and the pathophysiologic and biopsychosocial implications of pain
- To understand the somatic and visceral structures which contain receptors capable of creating pain
- To describe, at an appropriate level, the taxonomy of pain
- To differentiate acute and chronic pain and their proposed mechanisms
- To describe the anatomy, physiology, pathophysiology, and currently understood mechanisms of pain
- To describe the understood patterns of referred pain to and from the locomotor system
- To describe the relationship between psychosocial factors and chronic pain
- To describe the role of the autonomic nervous system in relation to pain
Integration af MM i den medicinske diagnostik:
SE, Den diagnostiske udfordring: 16 lektioner
Opfylder FIMM’s krav:
- To perform a conventional medical examination to understand the condition of the patient with respect to indications, contraindications and therapeutic options
- To perform thorough history and examination with emphasis on biomechanical, occupational, orthopaedic, neurological, biopsychosocial factors, to inspect posture, gait, and gross ranges of motion
- To perform orthopaedic, neurological, systemic and ancillary tests where indicated
- To prioritize diagnostic tests based on sensitivity, specificity and cost-effectiveness
- To describe practice guidelines or critical pathways in sequencing diagnostic evaluation for the patient.
Diagnostisering af dysfunktioner:
Nedenstående krav fra FIMM danner rammen om alle vore kurser.
Vi burger STAR (Sensory change, Tissue texture abnormality, Asymmetry, Range of motion) og MIP (Mobilisation, Irritation, Provocation) som mnemoteknik.
Rygkursus 3 lektioner
Ekstremitetskursus 8 lektioner
SE, Den diagnostiske udfordring 8 lektioner
MET A 3,5 lektioner
MET B 5 lektioner
CST-MFR B 2,3 lektioner
Idræts- og overbelastningsskader 3 lektioner
MET og Manipulation 2,5 lektioner
Masterkursus 4 lektioner
Opfylder FIMM’s krav:
- To perform screening examination to identify if there is a problem in the locomotor system that deserves additional evaluation
- To perform a scanning examination to identify which regions and tissues within the region are dysfunctional and of relevance at a level appropriate to the treatment skills
- To conduct regional palpatory examinations of the tissues of the locomotor system to identify dysfunctions
- To conduct palpatory examinations of local tissues to determine the specific dysfunctions considered for MM treatment and the characteristics important in the selection of the treatment modality including indications and contraindications
- To conduct different palpatory examinations in order to look at and record elements of pain provocation, sensory changes, tissue texture changes, examination of range of motion, and Characteristics of end‐feel barrier
Diagnostisk evaluering og re-test:
Rygkursus: 4 lektioner
Ekstremitetskursus 2 lektioner
MET A 1 lektion
MET B 1 lektion
CST-MFR A helt integreret
CST-MFR B 1,5 lektioner
Idræts- og overbelastningsskader 4 lektioner
Opfylder FIMM’s krav:
- To record the patient evaluation and patient progress by using various methods of measurement
- To record relevant specific findings in terms of MM medicine
Forudsat viden fra specialuddannelserne:
- To record pertinent related outcomes measures e.g. visual analogue scale (VAS), dolorimeter, impairment scales, general health scales
Behandlings principper:
Oversigt over de muskuloskeletale behandlingskoncepter, der i kursussammenhæng bliver gennemgået i DSMM-regi, beskrevet af Torben Halberg:
- Soft Tissue teknik
- Myofacial Release teknik (MFR)
- Mobilisation uden impuls
- Neuromuskulær terapi (Muskel Energi Teknik, MET)
- Mobilisation med impuls (HVLA, High Velocity Low Amplitude thrust technique)
- Integrerede teknikker (IFT, Indirect Functional Techniques)
Balance and Hold
Dynamic Functional Procedures. operator active
Dynamic Functional Procedures. operator passive
Release by positioning (Counterstrain)
- Osteopatiske behandlingsprincipper anvendt på kranierelaterede dysfunktioner
- Intra-Muskulær Stimulation (IMS)
Man kan groft inddele de forskellige behandlingskoncepter i de, der har behandlingsretning rettet direkte mod de restriktive barrierer, og de behandlingskoncepter hvor behandlingsretningen er bort fra de restriktive barrierer, enten hen mod det punkt hvor vævsspændingerne i alle tre bevægeplaner er mindst, mod det punkt der beskrives som ”pathologic neutral” eller ”dynamic balance point”, eller helt op mod de elastiske barrierer i de modsatte retninger af de restriktive barrierer.I en behandlingssekvens vil man ofte skifte mellem disse behandlingsprincipper for at opnå den hurtigste og mest skånsomme behandling af den enkelte patient. Det handler om at tilpasse behandlingsmetoden, så den er bedst for både behandleren og patienten. Rækkefølgen er vigtig fordi, man som behandler kun kan behandle med metoder man er fortrolig med, og som passer til ens hænder og temperament. Hvis ikke dette princip følges, vil det ikke føles rigtigt for patienten, og man kan ikke nå sit behandlingsmål. Jeg tror ikke, at nogle behandlingskoncepter er andre overlegne, men mere på samspillet mellem behandler og patient under behandlingen. Imidlertid vil en stor værktøjskasse være at foretrække, så man lettere kan tilpasse behandlingen til patienten og dennes problemer, og samtidig give behandleren en større frihed i sin behandling.Ofte anvendes i behandlingen release forbedrende tiltag (”Release Enhancing Maneuvers” / REM), hvor den kraftigste er åndedrættet. Ofte anvendes også øjenbevægelser eller bevægelse af enkelte dele af ekstremiteter. Den nedenfor beskrevne MET-teknik kan også anvendes som release forbedrende metode.
1: Soft Tissue teknik (bløddelsbehandling).
Metoden er defineret som en behandlingsprocedure rettet mod det myofascielle væv mere end mod selve skelettet. Man anvender den diagnostiske palpation til at monitorere de vævs- og mobilitetsændringer, der kommer. Konceptet opfattes som vævsmobilisering oftest rettet mod den restriktive/elastiske barriere. Der kan i behandlingsforløbet være elementer af traditionel massage, lineær eller tværgående stretching, tryk eller traktion.
2: Myofacial Release teknik (MFR).
Behandlingskonceptet hviler på den antagelse, at øger man hypertoniciteten ved dysfunktionen, vil den samlede neuromuskulære aktivitet kunne blive så stor, at impulsstrømmen brat stopper, og der optræder kortvarig lokal atoni (Release-fænomenet).
Dysfunktionen ophæves ofte herved.
Konceptet beskrives som BBR-Konceptet:
- Man skaber Balance i området over dysfunktionen
- Man skaber bevægelse hen mod den restriktive barriere, hvor man øger belastningen ved at øve let traktion og twistning af vævet
- Man venter på at Release vil indtræde i løbet af 10 - 30 sec.
Værktøjet man anvender, er et håndgreb, hvor man placerer sine hænder over dysfunktionen (vores "Point of entry") således at man kan opbygge "de 3 T-er":
- En Tension i vævet
- En Traktion
- En Twistning af vævsstrukturen under ens hænder mod eller bort fra den restriktive barriere
Ophæves en dysfunktion, vil ændringen skabe normal funktion i de tilstødende områder, og således, som ringe i vandet, kunne genskabe symmetrisk funktion af hele det muskuloskeletale system i postural balance.
Det er en teknik, der indeholder elementer fra de fleste osteopatiske behandlingskoncepter. Metoden beskrives ofte som en direkte behandlingsmetode, hvor man arbejder op mod den restriktive barriere. Man regner med, at behandlingseffekten er bedst i dette tilfælde. Imidlertid kan metoden også beskrives som en indirekte metode, hvor man arbejder bort fra den restriktive barriere, enten hen mod den modsatte elastiske barriere, eller hen mod punktet med mindst vævsspænding. I det sidste tilfælde skiftes behandlingskonceptet til det nedenfor beskrevne under de indirekte funktionelle teknikker.
3: Mobilisation uden impuls (artikulationsbehandling).
Behandlingsretningen er her hyppigst rettet mod den restriktive barriere, men her kan man også anvende en retning mod den elastiske barriere der ligger længst borte fra den restriktive barriere. Grænsen mellem mobilisering og manipulation vil af mange opfattes som hårfin, idet det bliver et spørgsmål om, man ved mobiliseringen flytter den restriktive barriere så langt, at man også behandler det hæmmede led ud i det parafysiologiske rum.
4: Neuromuskulær terapi (Muskel Energi Teknik, MET).
Teknikken beskrives som en aktiv direkte teknik, der arbejder direkte mod den restriktive barriere.
Kraften i behandlingen er intrinsic (ydet af pt. selv).
MET er defineret som en manuel medicinsk behandlingsteknik, hvor pt. efter behandlers anvisning:
- aktiverer sine muskler, til en bevægelse i en bestemt retning
- med en kraft, der anvises af behandleren
Indenfor de neuromuskulære terapiformer beskriver man ofte 3 forskellige metoder:
- Mobilisation ved brug af direkte muskelkraft
- Mobilisation ved brug af post-isometrisk relaksation af agonister
- Mobilisation med reciprok inhibition af antagonister
Muskelkraften der anvendes er enten isometrisk (ca. 90%) eller isotonisk (ca. 10%).
Man anvender overvejende isometrisk muskelkraft i behandlingen af de dysfunktioner, hvor muskulaturen spænder hen over det dysfungerende område. Dette gælder hovedsagelig for dysfunktioner i columnas led.
Den isotoniske muskelkraft anvendes hyppigst i de tilfælde, hvor muskulaturen ikke spænder hen over dysfunktionen.
Dette gælder især for dysfunktioner i pelvis.Konceptet beskrives altså som en direkte behandlingsmetode, hvor behandlingsretningen er rettet mod den restriktive barriere. Imidlertid vil man ofte med fordel kunne skifte mellem denne direkte behandlingsmetode og de nedenfor beskrevne indirekte funktionelle teknikker, hvor man så primært opfatter MET som en release forbedrende manøvre.
5: Mobilisation med impuls (manipulations-behandling, "High Velocity, Low Amplitude, Thrust Technique").
Behandlingsformen er her oftest beskrevet som en direkte behandlingsform mod den restriktive barriere. Behandlingen foregår i det parafysiologiske rum. Man påfører vævet lille belastning med stor hastighed op mod den restriktive barriere, uden dette udløser smerter. Belastningen appliceres dog forskelligt alt efter hvilken forklaringsmodel der lægges til grund for behandlingen.
I Nordamerika, England og Midteuropa diagnosticerer man ændret funktion. Man diagnosticerer dysfunktionen ved at lokalisere ændringerne i de segmentære bevægemønstre. Der er ved en hæmmet bevægelse antagelig opstået en restriktiv barriere og et deraf følgende funktionstab. Dette er ofte beskrevet som ophævet “Joint Play”. “Joint Play” er defineret som den lille bevægemulighed, et led skal have mellem den elastiske barriere, der er grænsen for den passive bevægemulighed, og den anatomiske barriere, der er grænsen for den maksimale bevægemulighed. (John Mennell). Man applicerer behandlingskraften direkte mod den/de restriktive barrierer ved dysfunktionen. Behandlingen må aldrig foregå i en retning, der udløser smerter. Behandlingsretningen kan også rettes modsat bevægehæmningen. Manipulationen beskrives da som en indirekte eller “Rebound”-manipulation. Denne metode kan anvendes, hvis behandlingsretning mod barrieren er smertegivende, mens den modsatte retning er smertefri. (J.F. Bourdillon)
Mange amerikanske osteopatiske behandlere mener, at man ikke skal anvende mobilisation med impuls-teknikken, hvis man ikke kan behandle direkte mod den restriktive barriere. De anbefaler i stedet at anvende en af de øvrige manuelmedicinske behandlingsteknikker.
I Frankrig og andre latinsktalende lande diagnosticeres det smertegivende område, idet man her forestiller sig , at smerten forårsage dysfunktionen. Man manipulerer altså kun smertegivende dysfunktioner, og kun, hvis der findes en smertefri behandlingsretning. Manipulationen udføres altid modsat den retning, der udløser smerte eller patientens symptomer. Det kaldes “reglen om ingen smerte og modsat bevægelse” defineret af R. Maigne. Manipulationen vil ofte her være en indirekte manipulation. Det er af R. Maigne anført, at en manipulation bedst kan gennemføres, hvis der er 3 ud af de 6 mulige bevægeretninger, der er smertefrie Han anfører, at manipulationen kan gennemføres med ca. 70% sikkerhed, hvis der kun er 2 smertefrie bevægeretninger, mens der kun er maks. 40% sikkerhed, når der kun er én smertefri bevægeretning. I dette sidste tilfælde fraråder han manipulation.
Min erfaring er, at hvis man manipulerer, kan man med stor fordel skifte mellem den direkte og den indirekte metode, Man skal også efter min mening undlade at manipulere to gange efter hinanden i samme behandlingsretning. Dette mindsker risikoen for manipulationsskader.
Man skal huske, at thrustbehandlingen skal rettes mod det restriktive væv, der både kan være det hypertone væv eller den dysfungerende facet ved bevægesegmentet, og ikke specielt fokusere på at frembringe en manipulationslyd. Ifølge Sutherland er den perfekte manipulation ”noiseless”.
6: Integrerede teknikker (indirekte funktionelle teknikker).
De forskellige indirekte behandlingsmetoder arbejder alle bort fra den restriktive barriere hen mod det punkt, hvor vævsspændingen i alle bevægeplaner er mindst. Punktet kaldes ofte ”Dynamic Balance Point” (DBP), ”Dynamic Membraneus Point” (DMP) eller ”Balanced Membraneus Tissue” (BMT).
Herfra kan forskellige behandlingsstrategier anvendes.
- Balance and Hold
- Dynamic Funktional Procedures. Operator Active
- Dynamic Funktional Procedures. Operator Passive
- Release by Positioning
Ad. 1: Ved denne metode holdes strukturen på DBP i 5-30 sek., hvor respirationen sætter grænsen. Uden anvendelse af respirationen kan DBP holdes i 30-90 sek., hvorved teknikken har meget fælles med princip 4. Proceduren gentages et antal gange. Man vil hele tiden finde det nye DBP nærmere det normale balancepunkt for vævet. Behandlingen slutter når man har genskabt normal bevægelse.Ad. 2: Fra DBP forsøger behandleren at "tilbyde" en lille bevægelse i forskellige retninger. Da bevægelsesindskrænkningen er forskellig i de forskellige retninger, vil man kunne "guide" vævet gennem de bevægemønstre som tillades, uden der opstår væsentlig modstand fra de omgivende strukturer indtil vævets normale bevægemønster er genskabt.Ad. 3: Fra DBP følger behandleren passivt, efter han har introduceret en lille bevægelse, de bevægelser i forskellige retninger som vævet selv ønsker at foretage for at genskabe sit normale bevægemønster. Disse bevægelser kan beskrives som en "Unwinding" (G.A. Laughlin, E. Stiles).Ad. 4: Denne teknik blev primært beskrevet af Lawrens Jones som teknikken ”Strain-Counterstrain”, senere alene ”Counterstrain Technique”.
Hans definition af metoden er følgende: ”Strain-Counterstrain-metoden kan lindre eller fjerne en smerte i columna eller andre led, ved at behandleren passivt anbringer leddet i den stilling, der for leddet føles mest komfortabel, eller at opnå det samme ved at mindske eller standse den fortsatte uhensigtsmæssige proprioceptive aktivitet i det afficerede område ved at tilstræber en betydelig forkortelse af den muskel, der indeholder den dysfungerende muskelspindel ved hjælp af en let belastning af denne muskels antagonist”.
Med denne teknik skal behandleren monitorere en række" tenderpoints" (defineret af Jones) mens han samtidig anbringer patienten i den stilling, hvori han kan monitorere mindst ”tenderness” i vævet. Denne stilling fastholdes i 30-90 sek. Det er den eneste teknik hvor man lader sig lede af den ”tenderness”, der registreres i det hypertone væv.
Ofte vil dette punkt også være det punkt, hvor vævstensionen er mindst, og man kan også lade sig vejlede at dette. Hvis man gør dette, skifter man fra det oprindelige ”Jones-princip”, og man vil herefter finde fællestræk med princip 1.
7. Osteopatiske behandlingsprincipper anvendt på kranierelaterede dysfunktioner.
Artikulationerne mellem craniets forskellige knogler er overvejende syndesmoser, men kan også som artikulationen mellem os occipitale og os sphenoidale være en synchrondrose.
Konceptet hviler desuden på den antagelse, at der hele livet bevares en vis bevægemulighed og dermed en lille bevægelse mellem craniets forskellige knogler og sammenhængende strukturer.
(W. G. Sutherland)
Hæmmes denne bevægelse er der skabt en dysfunktion. Ved palpation vil der i normale tilfælde kunne registreres en svag rytmisk bevægelse, hvis frekvens er mellem 6 og 14 svingninger pr. min. Man beskriver en amplitude på 0.38mm –1mm. Disse svingninger vil via det meningeale system forplante sig til den øvrige del af kroppen. En hæmning af denne bevægemulighed, enten lokalt i craniet eller mere generelt, vil medføre symptomer, der enten kan optræde lokalt svarende til det dysfungerende område eller være mere generelle, ofte med udbredelse til helt andre regioner. Man vil i disse tilfælde registrere en ændring af den ovenfor anførte frekvens enten som færre eller som flere svingninger pr. min. Dette kan registreres enten lokalt ved dysfunktionen eller mere generelt.
Bevægelsen der skabes, kan i princippet palperes overalt på kroppen, men kan tydeligst palperes over kraniet og over sacrum (pga. dura maters insertion). Uanset hvor i kroppen der optræder dysfunktioner, vil disse forstyrre denne bevægelse, og man vil registrere en ændring i rytme eller bevægeretning for de strukturer, der palperes.
Et ændret bevægeudslag eller en ændret rytme palperet over kraniet kan være sekundær til dysfunktioner i andre regioner, hvilket i øvrigt er det hyppigst forekommende, men de kan også være en direkte følge af et kranietraume og dermed en primær craniel dysfunktion. Kun i det sidstnævnte tilfælde kan man overveje at behandle de cranielle dysfunktioner primært, men ofte er der i skadeøjeblikket også opstået dysfunktioner i andre regioner, og de skal altid behandles først.
Foreligger der ikke et direkte kranietraume, skal alle dysfunktioner i andre regioner primært behandles. Først herefter kan den cranielle rytme vurderes og behandlingsbehovet over kraniet registreres.
Ved dysfunktioner vil man normalt registrere svingninger mellem det frie “still point” og det “still point”, der findes ved den restriktive barriere.
Ved den funktionelle indirekte teknik vil man følge vævets svingninger bort fra den restriktive barriere mod det frie “still point”. Vævet holdes kortvarigt i dette punkt (sekunder til få minutter) og følges i den næste svingning. I “still point” kan man med en let kraftpåvirkning (få gram til max. 500 gram) ændre retning i vævets svingning. Proceduren gentages til den restriktive barriere undviges, og release opstår, hvorefter barrieren ofte “smelter” bort.
I nogle tilfælde vil man vælge den funktionelle direkte teknik hvor man først følger vævet mod “still point” ved den restriktive barriere og holder vævet kortvarigt i dette punkt, før man følger vævet i den næste svingning. I “still point” kan en let kraftpåvirkning ændre vævets svingning. Proceduren gentages, til release optræder.En anden behandlingsteknik, der kan anvendes, er ”Myofascial Release Technique”.
Denne teknik kan anvendes enten som indirekte teknik, hvor vævet føres bort fra den restriktive barriere til den indirekte barriere, eller som den direkte teknik, hvor vævet føres direkte mod den restriktive barriere. I begge tilfælde påføres vævet en kraft ved den engagerede barriere (tension, traktion og twistning af vævet), indtil der optræder release i vævet, og barrieren “smelter” bort.
Generelt kan siges at man ved de indirekte teknikker skal anvende mindre kraft end ved de direkte teknikker.
Et acceptabelt behandlingsmål er 50% reduktion af dysfunktionen.
Man kan facilitere ved hjælp af åndedrættet.
8: Intra-Muskulær Stimulation (IMS) eller blokadebehandling.
Disse behandlingsmetoder kan anvendes som supplerende behandlingsmetoder til de andre osteopatiske teknikker, eller som eneste behandlingsmetode i et behandlingsforløb, ligesom akupunktur kan anvendes til behandling efter behandlerens eller patientens aktuelle ønske eller behov.
Rygkursus
Mobilisation uden impuls, introduktion til MET 12,5 lektioner
Ekstremitetskursus
Mobilisation uden impuls, introduktion til MET 17 lektioner
MET A 15 lektioner
MET B
MET 19 lektioner
HVLA 5 lektioner
MET og Manipulation
MET 16 lektioner
HVLA 15 lektioner
CST-MFR A
CST 12 lektioner
MFR 6 lektioner
CST-MFR B
CST 12 lektioner
Indirekte Funktionel Teknik 1 lektion
MFR 3 lektioner
Idræts- og overbelstningsskader
Mobilisation uden impuls, MET 3 lektioner
Masterkursus
All behandlings principper 18 lektioner
Opfylder FIMM’s krav:
- To conduct mobilisation techniques including specific techniques for muscle inhibition or muscle relaxing (muscle energy techniques, techniques based on post isometric relaxation and on reciprocal inhibition, and positioning techniques)
- To conduct segmental manipulation techniques of the spine and the peripheral joints
- To supervise or monitor physiotherapy and training for rehabilitation
- To conduct myofascial techniques
- To conduct trigger point therapy
- To apply treatment strategies for interlinked functional (chain reaction) syndromes
- To integrate the principles of treatment of MM medicine into multimodal treatment concepts
Øvelsesbehandling og forebyggelse af tilbagefald:
Rygkursus: 2 lektioner
Ekstremitetskursus 4 lektioner
CST-MFR B 1 lektion
Idræts- og overbelastningsskader 14 lektioner
Opfylder FIMM’s krav:
- To use all treatment modalities to prevent recurrence of presenting problems in MM medicine
- To maximise biomechanical and physiological functions in activities of daily living, in activities in work and in sports
- To recommend exercise and sound ergonomic behaviour for rehabilitation and prevention
MM tilgang til Kliniske billeder og syndromer:
Rygkursus 2 lektioner
MET A 3,5 lektioner
MET B helt integreret
CST-MFR A 2,0 lektioner
CST-MFR B helt integreret
Idræts- og overbelastningsskader 9 lektioner
Opfylder FIMM’s krav:
- Disorders or dysfunctions of axial and appendicular structures:
- cranium
- Cranio-cervical junction
- cervical spine
- cervico-thoracic junction
- Thoracic spine
- thoraco-lumbar junction
- Lumbar spine
- lumbo-sacral junction
- Sacroiliac joints
- Pelvic girdle
- Peripheral joints
- Visceral organ dysfunction related to biomechanical disorders
- Viscera-somatic, somato-visceral, psycho-somatic and somato-somatic reflexes
- To understand the differential diagnosis, relevance and interrelationship to MM medicine of the following:
- general neurological semiology (signs and symptoms)
- neurological disorders
- headache due to metabolic pathologies
- rheumatologic disorders
- spinal affections
- vascular abnormalities
- paediatric disorders
- trauma of the spine
- tumours of the spine
- To understand special consideration with respect to age and development (esp. Paediatrics and geriatrics)




